As the UK nears what will hopefully be the end of lockdowns and high death tolls, our doctors and nurses are left to deal with a worrying secondary aspect of the pandemic in the shape of long Covid. There are more than 1 million people with long Covid in the UK alone, amounting to a human and medical emergency, with potentially a huge impact on society and the workforce. A clinical picture is emerging, with many patients reporting similar symptoms including shortness of breath, difficulty in concentration, body aches, persistent fatigue and other symptoms. The illness has been recognised in the US, Europe and elsewhere. Moreover, long Covid has parallels with CFS/ME, a debilitating condition that has similar symptoms.
Unfortunately, in the face of all this suffering, advances in science and clinical care are being jeopardised by an antiquated and unhelpful debate on whether these symptoms are “in the mind”, as if they were a fantasy or a dream. Of course, long Covid and CFS/ME symptoms are not in the mind. No symptoms are. Unfortunately some people with CFS/ME or, more recently long Covid, have been dismissed by health professionals. Some patients might have felt not taken seriously by their doctor while others might have lost the opportunity to benefit from a broader, psychosocial approach.
I am a medical researcher and clinician who specialises in the biological communication between the body and the brain. I can assure you that every symptom and every disorder, regardless of whether it is called mental or physical, is characterised by measurable biological changes in the body and in the brain. We may not know yet if these changes are the cause of the symptoms, but these biological changes are very real even if we cannot fully understand them.
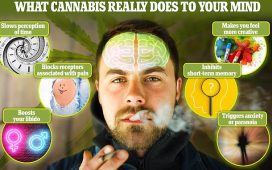
Interestingly, the same biological mechanisms can often be triggered by diverse events. Both life events and infections activate the immune system, with common effects on the brain and the body, resulting in both depression and fatigue. It is not at all surprising that most patients with CFS/ME recognise either a severe life event or an infection at the onset of their illness.
Indeed, even the historical distinction between a mental and a physical disorder is fuzzy when we look at individuals rather than clinical labels. This distinction was never intended to explain the cause of a disorder but rather to describe its main manifestations: that is, abnormal emotions or behaviour for mental disorders versus abnormal functions of the heart, the lungs or other organs for physical disorders.
Moreover, mental and physical disorders are often present together in the same person. Many people with cardiovascular disease and diabetes also have depression, and there are many other similar combinations of diseases. Mental disorders, such as anxiety, depression, schizophrenia or bipolar disorder, have measurable biological changes not only in the brain but also in the body: changes in the blood, saliva and urine, in the heart and the digestive systems. The idea that there is a clear mental health versus physical health distinction has changed in recent years toward treating the health of the person as a whole.
The fact that all symptoms and disorders have underlying biological changes does not diminish the strong evidence that symptoms and disorders can be influenced by “psychological factors”. Many people fully acknowledge that our health can be influenced by what happens in our lives and how we feel about those things – both negative and positive.
Stressful life events, such as bereavement, unemployment, incidents of abuse and violence, poverty or discrimination, can precipitate or exacerbate both mental and physical disorders. These events can lead to hypertension, an autoimmune flare-up, a cardiovascular problem or depression. Why would we want to separate these health impacts and put depression, or any mental disorder, in a separate box to the rest?
Conversely, changes in lifestyle and behaviour, and psychological therapies (which work by challenging unhelpful ways we think about ourselves and world around us), have been shown to help patients with physical disorders including cancer, irritable bowel syndrome, diabetes, multiple sclerosis and stroke, to name just a few.
This point is particularly important in the context of CFS/ME and, more recently, long Covid. Offering lifestyle changes or psychotherapeutic approaches to these patients does not mean that their symptoms are “not real”. Medics routinely help cancer patients with these approaches every day, yet I never hear anyone accusing doctors of suggesting cancer is all in the mind.
There is also good evidence that all types of symptoms can be influenced by anticipation and beliefs, as has been demonstrated many times with the powerful placebo and “nocebo” effects. Being offered something believed to be positive (for example, an empty capsule that we believe to contain a medication) or negative (an empty capsule we believe to contain a toxin) will make our symptoms better (placebo) or, respectively, worse (nocebo). This is not snake oil for the gullible: these are biological effects based on measurable changes in the brain and the body, and can occur in everybody. This is why the standard evaluation of a novel treatment for any disorder – including the very real Covid infection – requires a comparison with a dummy treatment, so that our expectations, positive or negative, do not influence the results. This concept is particularly relevant in the context of the recent controversy around a Guardian article on this topic, and the response it has received.
Patients being told their symptoms are in their mind is completely unacceptable to every doctor I know, and such attitudes have no place in modern medicine. But this dismissive approach has nothing to do with the important clinical understanding that psychological factors and approaches can influence these conditions, as they do any other illness. Those who reject the notion that psychological approaches can help us better understand and treat physical symptoms are themselves falling, perhaps inadvertently, into the trap of differentiating and stigmatising mental illness.
We need every tool in the box to treat long Covid – and it must be hoped that the new focus and funding on this condition may also provide us with new and useful insights into treating CFS/ME patients.